OBSTETRIC BRACHIAL PLEXUS PALSIES (OBPP)
from: McGuinness & Kay. Current Orthopaedics. 13:20-26. 1999.
Incidence is approx 2/1,000 births
Risk Factors:
Child
weight > 4000g / large for gestational age
Maternal
multiparity
diabetes
sibling with shoulder dystocia or OBPP
At Birth
shoulder dystocia
breech
long labour
forceps delivery.
Investigations:
EMG - doesn't correlate with prognosis & can be misleading.
MRI - fast spin echo MRI may demonstrate root avulsions.
Classification Table:
TYPE (Adler & Patterson) | TYPE (Narakas) | ROOTS | DEFICIT | PROGNOSIS |
Erb-Duchenne | Group 1 | C5,6 | Deltoid, cuff, elbow flexors, wrist & hand dorsiflexors - 'waiters tip' | Best |
Group 2 | C5-7 | Above except with sightly flexed elbow | Poor | |
Klumpke | C8-T1 | Wrist flexors, intrinsics, Horners | Poor | |
Total Plexus | Group 3 | C5-T1 | Sensory & motor, flaccid arm | Worse |
(Total Plexus + Horners) | Group 4 | C5-T1 | Sensory & motor, flaccid arm, Horner | Worst |
Natural History:
C8-T1 injury with a Horners syndrome has the worst prognosis.
Isolated lower root lesions have a poor prognosis, since they are usually avulsion injuries.
The rate of recovery and the time of beginning of recovery affect the outcome.
Toronto scoring system (Clarke) assesses the child at 3 months of age
No biceps function at 3m indicates a poor prognosis.
Patients who show evidence of biceps function before 6 months of age have near-normal to excellent function.
In borderline cases exploration of the Brachial Plexus is performed.
Early repair has the best prognosis.
Recovery continues until 1 year old, then little further recovery thereafter.
Management:
Early Referral to a specialist unit.
Physiotherapy - passive range of motion exercises.
Splinting - not popular.
Surgery
Indications for Surgery:
C8-T1 injury with a Horners syndrome
C5/6 lesions with no muscle activity & breech baby.
Toronto score <>
Failure to progress adequately between 12-24 weeks
EMG criteria of Smith where doubt exists.
Surgical Technique:
Transverse incision
Neurolysis
Nerve grafting (Sural nerve)
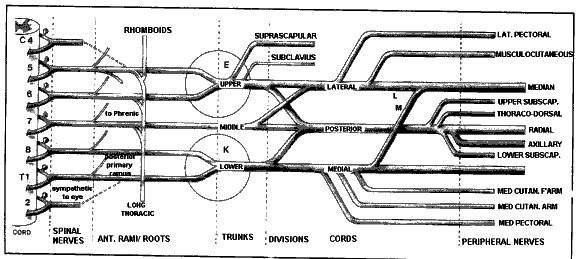
Nerve transfers (accesory to suprascapular, intercostal to musculocutaneous)
Late Deformities:
Internal rotation & adduction contraction of the shoulder
modified L'Episcopo procedure - involves lengthening of pectoralis major & subscapularis tendons with transfer of teres major & insertions into posterior surface of the humerus to act as external rotators
osteotomy - for older children with fixed bony adaptive changes, proximal humeral external rotation osteotomy can be considered; - these patients will most often complain of internal rotation contracture
Posterior glenohumeral subluxation: - limitation of external rotation; - in late cases, with a deficient posterior glenoid consider humeral derotational osteotomy.
TORTICOLLIS
from fibrosis of sternal head of sternocleidomastoid
can result from unilateral shortening of sternocleidomastoid, commonly associated with fibrosis of the muscle; (may also involve the platysma and scalene muscles)
Aetiology & Natural History
birth trauma, occlusion of venous flow, or haematoma results in fibrosis of muscle & palpable mass noted within first 4 weeks of life
mass usually resolves within the first year of life (90% resolve)
non-tender enlargement may be palpated in body of sternocleidomastoid
Grisel's Syndrome:
Atlantoaxial Rotary Subluxation in association with pharyngeal infection, occurs predominantly in children
it results in severe torticollis, resistant to manual therapy
> 5 mm of anterior displacement of arch of C-1 (Fielding type III) indicates disruption of both facet capsules as well as transverse ligament
reduction w/ skeletal traction, followed by atlantoaxial fusion, is recommended
Rigid Torticollis:
may also present as rigid deformity, & sternocleidomastoid is not contracted or in spasm
torticollis most often follows an injury to the C1-C2 articulation; - frx of the odontoid in young child may not be apparent on initial x-rays
Associated Anomalies:
congenital atlanto-occipital abnormalities
bony anomalies of the Cervical Spine, esp involving C1 & C2
congenital webs of skin along the side of the neck, pteygium colli
DDH: (20%
plagiocephaly: - w/ persistent contracture of sternocleidomastoid, deformities of face and skull result and are apparent within first year of life; - flattening of face is noted on side of contracted sternocleidomastoid and is probably caused by child's sleeping position
metatarsus adductus
opthalmic disorders causing the child to tilt the head.
Non Operative Treatment:
90% will respond to passive stretching within the first year of life
in first yr of life, rx consists of stretching sternocleidomastoid muscle by trying to rotate the head to opposite position. - stretching exercises should include not only lateral rotation, but also side bending to the opposite shoulder
Indications for Surgery:
failure of non operative treatment after 12 to 24 months of age, surgical intervention is needed to prevent further facial deformity
Operative Treatment:
involves resection of portion of distal sternocleidomastoid muscle from its sternal and clavicular attachments through transverse incision in the normal skin fold of the neck
skin incisions immediately adjacent to clavicle may result in unsightly hypertrophic scars. - transverse skin incisions in skin folds 1.5 cm proximal to clavicle result in imperceptible scars
uncommonly, distal resection is insufficient and proximal release of sternocleidomastoid is needed;


1 komentar:
I'd like to take the power of thanking you for that specialized guidance I've constantly enjoyed viewing your blog.
a knockout post
Posting Komentar