from: Hardcastle & Nade. JBJS(B): 67-B(5):741-6
As a result of our observations, we have formulated a standard method of performing the Trendelenburg test; if this is used the response can be interpreted in a clinically meaningful way. To perform the test properly does take time, and its accurate assessment demands the full understanding and co-operation of the patient.
How to do the test
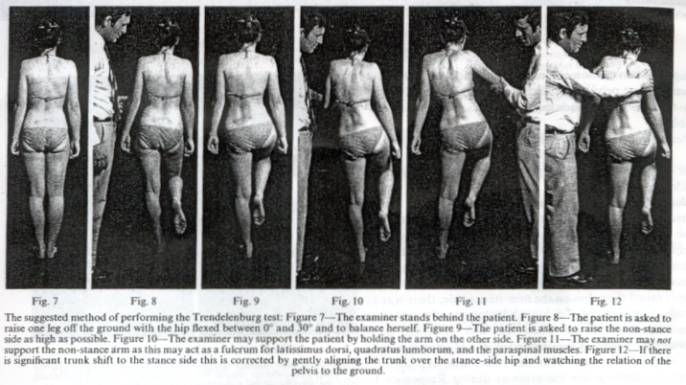
1. The examiner stands behind the patient and observes the angle between the pelvis (the line joining the iliac crests) and the ground (Fig. 7).
2. The patient is asked to raise from the ground the foot of the side not being tested, holding the hip joint at between neutral and 30 of flexion. The knee should be flexed enough to allow the foot to be clear of the ground in order to nullify the effect of the rectus femoris muscle. The position of the pelvis is again noted (Fig 8) A supporting stick can be used in the hand only on the side of the weight-bearing hip; alternatively, both shoulders can be supported by the examiner so as to maintain balance without a stick (Fig. 12).
3. Once balanced, the patient is then asked to raise the non stance side of the pelvis as high as possible (Fig 9). The examiner may support the patient by holding the arm on the stance side (Fig 10; compare with Fig. 11)
4. If the patient leans too far over to the side of the weight-bearing hip, the examiner corrects this by gentle pressure on the shoulders to bring the vertebra prominens approximately over the centre of the hip joint and the weight-bearing foot (Fig. 12).
Interpretation
(a) The response is NORMAL (i.e. the test is "-negative") if the pelvis on the non-stance side can be elevated as high as hip abduction on the stance side will allow, and providing this posture can be maintained for 30 seconds with the vertebra prominens centred over the hip and foot.
(b) The response is ABNORMAL (i.e. the test is "positiveâ€) it' this cannot be done. This includes responses where the pelvis is elevated on the non-stance side above the stance side, but where this elevation is not maximal.
(c) The response is also ABNORMAL if the pelvis can be lifted on command, hut can not be maintained in that position for 30 seconds. The time taken before the pelvis starts to fall is recorded. By introducing a time ele-ment, the Trendelenburg test can be objectively recorded for comparison purposes. Obviously the response described in (b) constitutes a zero time Trendelenburg test.
Non-valid responses. In the presence of back or leg pain or of deformity, or if the patient is uncooperative because of age or mental status, inappropriate responses may arise (Table II). An abnormal response (positive test) in these circumstances can be misleading. However, if the test is negative that is significant-it means that the subject does not have abnormal hip mechanics
Significance
Neurological disorders. MRC Grade 5 abductor muscle strength was required to produce a normal response. All subjects whose hip abductor power was Grade 4 or less had abnormal responses at times between 0 and 25 seconds. Some patients in this group were able to elevate the pelvis, but not to the full extent. We considered this to be a positive Trendelcnburg test at 0 seconds.
One subject who had Grade 5 strength on clinical testing had a delayed (or timed) positive Trendelenburg test at 15 seconds. Only one subject with Grade 3 hip abductors had an initial negative response which became positive at 5 seconds (a delayed positive test). He had a good rectus femoris muscle which probably helped. The two subjects with isolated nerve root entrapment of L5 or SI had negative responses.
Mechanical disorders.
Congenital dislocation of the hip. The Trendelenburg test was always positive in subjects with congenital dislocation of the hip. One patient who had been treated by bilateral replacement arthroplasty had a normal response when examined three years after surgery.
S ubl uxating hips. Mitchell (1973) has described the importance of the delayed (timed) Trendelenhurg test in assessing clinical deterioration in adolescents with acetabular dysplasia. Our two patients with subluxating hips both had positive (timed) Trendelenburg tests, one at 15 and one at 20 seconds.
Coxa vara. The test may be positive or negative depend-ing on the femoral neck angle and the presence of degenerative changes. With femoral neck angles of up to 100 degrees the response can be normal. One child with an angle of 90 after a varus osteotomy had a positive test at 20 seconds.
Slipped femoral capital epiphysis. The Trendelenburg test was not altered by the rotation of the femoral head in relation to the femoral neck and the subjects examined all had negative responses if they were pain free.
Perthes disease. The Trendelenburg test was not altered by the size of the femoral head. However, if there is incongruity or hinge abduction the test can become posi-tive, and a delayed positive response was seen in one subject.
Arthritis of the hip. Variable responses were observed but the type of response did not vary in the same individual when studied at different times. Obviously pain or progression of the disease would be expected to alter the response, particularly in respect to reduction of time of the normal response.
Leg length inequality after hip arthroplasty. Two patients with up to 2cm of shortening above the intertrochanteric line after hip replacement had negative Trendelenburg tests (i.e. normal responses).
Avulsion of the greater trochanter after hip arthroplasty. In the absence of pain, the Trendelenburg test was particularly valuable some time after operation. Where the osteotomy gap was greater than 2 cm the Trendelenburg test was positive either immediately (zero time) or with a delayed positive response.
Fractured neck of femur. Patients who had unstable fixation with Ender or Zickel nails had a positive response until the fracture was united radiologically. These people were tested initially 8 to 10 weeks after operation and had no pain at the time of their initial Trendelenburg response, which was positive. Two malunited fractures also had positive responses.
Avascular necrosis of the f e moral head. Hip pain made proper assessment of these cases difficult. However, one of our four patients had only mild symptoms; his test was positive at 20 seconds on the first examination, and at 25 seconds on the next day. In the other patients pain pre-vented adequate assessment.
Spinal disorders :
St i ffness. Totally stiff spines, as in ankylosing spondylitis, did not affect the test unless there was also abnormality of the hip or gross spinal deformity.
Deformity. Kyphosis did not affect the outcome. Severe scoliosis, however, may lead to impingement between the lower costal margin and the iliac crest and give a false-positive test.
Pain. Nerve root irritation can lead to false-positive results, but back pain itself did not lead to abnormal responses.
DISCUSSION
When asked to stand on one leg, and follow a standard routine to ensure hip abductor muscle contraction on the same side, patients may respond to the standardised Trendelenburg test in one of three ways. Only one response is normal; the other two are abnormal. An ability to assume the normal response must be absolute, and if the pelvis drops on the non-stance side within 30 seconds the Trendelenburg test is positive. The use of a timer is an essential part of the Trendelenburg test, and, indeed, makes it an objective measure of severity of altered hip mechanics.
However, the presence of pain, poor balance and either lack of co-operation or understanding by the patient can lead to false-positive tests, because the test cannot he properly performed. The reason for false-negative tests is that the subject uses muscles above the pelvis to elevate the non-weight-bearing side of the pelvis, or shifts the torso well over the weight-bearing side; these can be called "trick movementsâ€. Variable responses were noted in some patients less than seven years of age, and the test is of no value in children under four. Nevertheless, if the Trendelenburg test is carefully performed, it is an accurate clinical sign with prognostic implications.
Inman (1947) measured the torque strength about the hip with the pelvis in different postures with respect to the ground. Our electromyographic results confirm his findings that little abductor muscle strength/activity is necessary to maintain a balanced posture with the pelvis dropped (as in Response 3) on the non-weight-bearing side. As the pelvis rises on this side there is increase of abductor muscle activity provided that the torso is centred over the hip.
Functional assessment of a joint is important in the clinical assessment of patients. Observation of gait is probably performed less often than is desirable because of limitation of space. The Trendelenburg test allows for functional assessment in a confined space, and is a more valuable clinical sign than many static tests. It can also be easily recorded on film or videotape.
It is our belief that a patient who has an abnormal response to the Trendelenburg test as described in this paper has an inefficient gait, and therefore becomes easily fatigued. With a little practice, the test is not difficult to perform and interpret. Timing is an essential part of the test; it provides an objective measure of improvement or deterioration in the neuromuscular or mechanical function of the hip.
Trendelenburg's original observations were precise and clear, and his interpretations accurate. We support the need for meticulous clinical examination in order to provide correct diagnosis and we recommend the use of the standardised timed Trendelenhurg test in the assessment of function and malfunction of the hip.
Conclusions
1. The Trendelenburg test is a useful part of clinical examination if performed and interpreted correctly. We have described a standard method for performing the test.
2. False-positive and false-negative responses may occur, but their interpretation can be clarified if the test is properly performed.
3. The use of a timer when performing the test is essen-tial, and allows measurement of a "delayed abnor-mal" response.
REFERENCES
Inman VI. Functional aspects of the abductor muscles of the hip. J Bone Joint Surg~BrJ 1947;29:607-19.
Mitchell GP. The delayed Trendelenburg hip test. I nt Con gr Ser 1973; 291:1113.
Rang M. Anthology of orthopaedics. Edinburgh. E&S Livingstone, 1966; 139-43.


Tidak ada komentar:
Posting Komentar