By Elson, R. A.
JBJS - VOL. 68-B, NO. 2, MARCH 1986, pp. 229-231
From the Northern General Hospital, Sheffield
ABSTRACT: Closed rupture of the middle slip of the extensor hood of a finger is easily missed until the late appearance of a buttonhole deformity. Early diagnosis gives the best chance of satisfactory treatment, but Boyes' test becomes positive only at a late stage. A new test is described in which, from a 90 degrees flexed position over the edge of a table, the patient tries to extend the proximal interphalangeal joint of the involved finger against resistance. The absence of extension force at the proximal joint and fixed extension at the distal joint are immediate signs of complete rupture of the central slip. The theoretical basis and the method of performing the test are discussed. END OF ABSTRACT
Closed rupture of the central slip of the extensor tendon hood of the finger can easily be missed at an initial examination, even when it is suspected. Later, a classic buttonhole deformity will develop, but by then correction is difficult. Early diagnosis is essential for successful treatment. Boyes (1970) described a test for the integrity of the central slip. If the proximal interphalangeal joint is held passively extended, it is then possible for the normal individual to flex the terminal interphalangeal joint in isolation. However, if the central slip has been ruptured, there is increasing difficulty in performing this action. Unfortunately this test only becomes positive when the proximal part of the ruptured central slip has retracted and become adherent to the surrounding tissues. The test which is described below becomes positive immediately after complete rupture of the central slip.
Anatomy
The extensor mechanism of the human finger is complex, but its basic pattern is of three relatively uncompliant bands: one central slip and two lateral bands. These arise from the extensor communis tendon (Fig. 1). During flexion of a finger at both interphalangeal joints, the extensor hood mechanism moves distally, but the lateral bands must travel further than the central slip because they cross two joints. In addition, the finger lengthens during flexion because of the shape of the condyles of the middle and proximal phalanges, a point emphasised by Stack (1962). Harris and Rutledge (1972) demonstrated that, during flexion, the lateral bands sublux in a volar direction on either side of the head of the proximal phalanx, a movement facilitated by the conical shape of the bone. They also showed that during extension, the lateral bands recover their position on the dorsum of the finger and that this is not due to any elastic recoil from the triangular ligament. This could be divided; the lateral bands still returned to their dorsal position on extension provided that the central slip was intact (Fig. 2). Few individuals can flex the interphalangeal joints independently; this is because both flexor profundus and flexor superficialis act on the check-rein afforded by the extensor hood with its three uncompliant components. Action by the profundus tendon alone must take up the slack in the extensor hood as a whole and result in simultaneous flexion of both interphalangeal joints. Flexor superficialis acting alone must draw the hood distally, relaxing the lateral bands and allowing weak flexion of the distal joint by the normal tone of the flexor profundus. The well-known manoeuvre first described by Apley in 1956 demonstrates the integrity of flexor superficialis to one finger by neutralising the action of its profundus tendon and thus allowing the proximal interphalangeal joint to move in isolation.
Independent flexion of the distal interphalangeal joint can be achieved by holding the proximal joint in full extension. The action of flexor superficialis is blocked and flexor profundus can act on the distal joint alone (Fig. 3). When it does so, the lateral bands tighten, drag the extensor hood distally, and relax the central slip (which relates to the mechanism of Boyes' test). Some individuals with hypermobile proximal interphalangeal joints, can hyperextend and lock the joint in this position by the action of the central slip. They are then able to contract the profundus tendons to all the fingers and produce the unusual posture shown in Figure 4.
Theoretically, the oblique retinacular ligaments of Landsmeer (1949) should preclude flexion at the distal interphalangeal joint while the proximal joint is fully extended, but in practice, as shown above, this is not the case. Only later may contracture of the retinacular ligaments contribute to holding the lateral bands in subluxation; they play no effective part in the findings in acute injury. This was recognised by Harris and Rutledge (1972) and by Bendz (1985). The retinacular ligaments may therefore be neglected in describing the new test.
When the proximal interphalangeal joint is held at 90 degrees flexion the central slip is drawn distally and the lateral bands therefore become slack unless the distal joint is also flexed; this is easily demonstrated (Fig. 5), and it is in this posture that the new test is effective.
Test for integrity of the central slip.
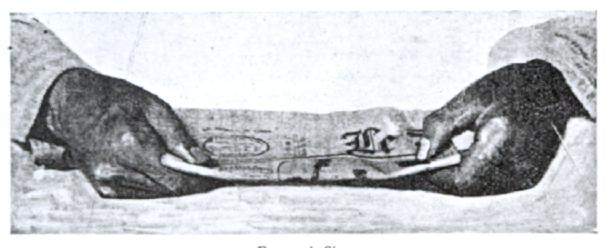
The finger to be examined is flexed comfortably at a right angle at the proximal interphalangeal joint, over the edge of a table and firmly held in this position by the examiner (Fig. 6). The patient is then asked to attempt gently to extend the proximal interphalangeal joint. Any pressure felt by the examiner through extension of the middle phalanx in the posture described can only be exerted by an intact central slip. Final proof is that the distal interphalangeal joint remains flail during this effort, since the competent central sip prevents the lateral bands from acting distally.
In the presence of complete rupture of the central slip, any extension effort perceived by the examiner will be accompanied by rigidity at the distal interphalangeal joint with a tendency to extension (Figs 7 and 8). This is produced by the extensor action of the lateral bands alone. This test will not demonstrate partial rupture of the central slip, and its performance may be impeded by pain or by lack of co-operation from the patient. Pain can be relieved, if necessary, by proximal infiltration of the dorsal nerves of the finger.
Boyes' test for rupture of the central slip uses a different mechanism. It depends upon retraction of the proximal end of the ruptured central slip and its adhesion to surrounding tissues, and will, therefore, not become positive until these adhesions have developed. Irrespective of the chosen method of treatment, it is clear that early diagnosis of complete rupture of the central slip is essential; this can be achieved by the test which has been described.
Article Figure Legends
FIGURE 1: Diagrams to show the central slip and one of the lateral bands arising from point X. Distal pull on the central slip relaxes the lateral band, while a distal pull on the lateral band relaxes the central slip. These effects can readily be demonstrated in a fresh dissection.
FIGURE 2: Diagram of the distal end of a proximal phalanx, to show the conical shape which facilitates volar displacement of the lateral bands during flexion of the proximal interphalangeal joint. During extension they move in the direction indicated by the arrows provided that the central slip is intact (modified from Harris and Rutledge 1972).
FIGURE 3: If the proximal joint is held extended by an examiner, isolated flexion of a normal distal interphalangeal joint is possible. This is not possible once adhesions have developed after a rupture of the central slip (Boyes' test).
FIGURE 4: In some individuals, hypermobility of the proximal interphalangeal joints allows them to lock into hyper-extension. The flexor profundus can then act in isolation on the distal joints. Locking is maintained by the bowstring tension induced in the lateral bands; in this position the central slip is relaxed because the lateral bands have pulled the extensor hood distally.
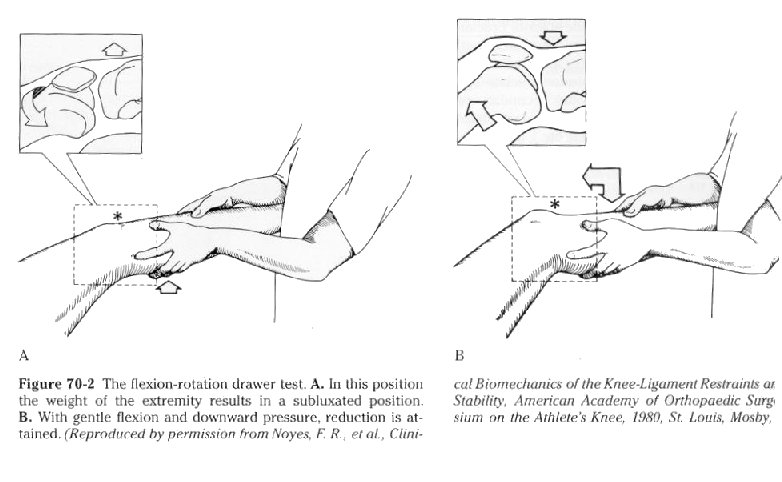
FIGURES 5 and 6: Diagram and photograph showing a normal proximal interphalangeal joint flexed passively to 90 degrees. The origin of the lateral bands is drawn distally by the intact central slip, which allows the distal joint to remain flail. Attempted active extension affects the middle phalanx but leaves the distal joint flail.
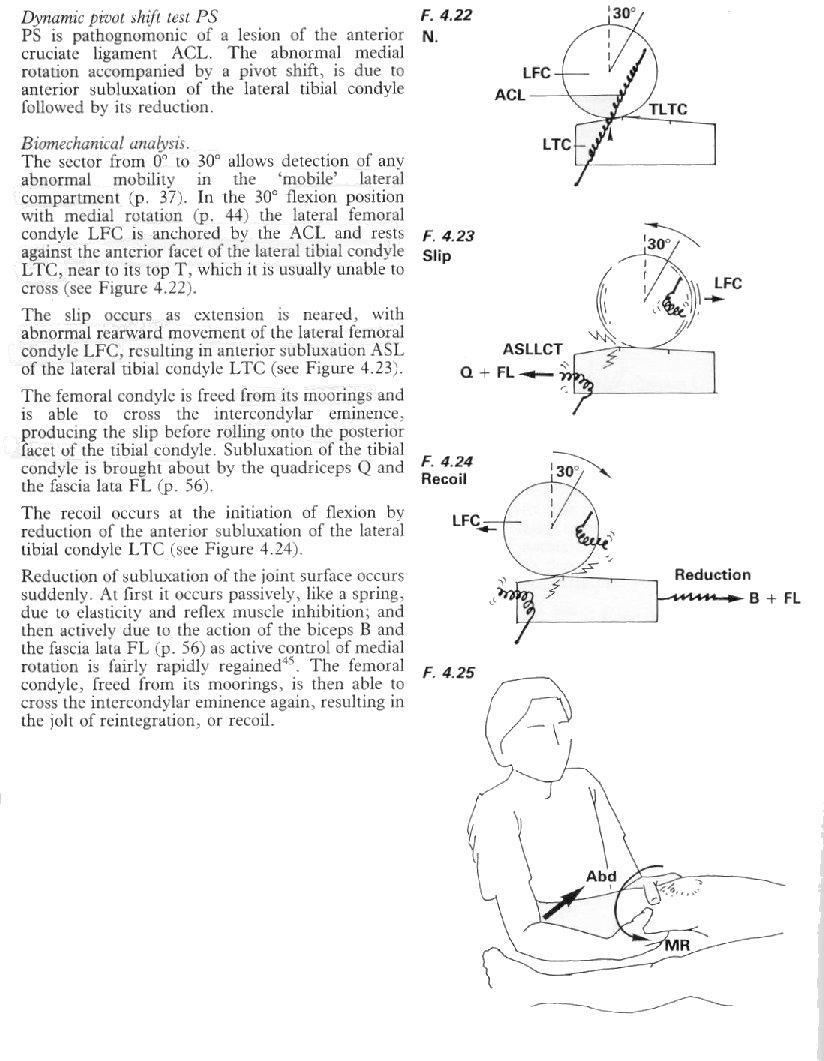
FIGURES 7 and 8: Diagram and photograph to show the effect of division of the central slip. This allows proximal movement of the origin of the lateral bands; they hold the distal joint in extension.
References
Apley AG. Test for the power of flexor digitorum sublimis. Br Med J 1956;i:25-6.
Bendz P. The functional significance of the oblique retinacular ligament of Landsmeer: a review and new proposals. J Hand Surg 1985;10-B:25-9.
Boyes J, reviser. Bunnell's surgery of the hand. 5th ed. Philadelphia: JP Lippincott, 1970:440-1.
Harris C Jr, Rutledge GL Jr. The functional anatomy of the extensor mechanism of the finger. J Bone Joint Surg [Am] 1972;54-A:713-26.
Landsmeer JMF. The anatomy of the dorsal aponeurosis of the human finger and its functional significance. Anat Rec 1949;104:31-44.
Stack HG. Muscle function in the fingers. J Bone Joint Surg [Br] 1962;44-B:899-909.